Usher Syndrome Awareness Day is Sept 18. You might not have heard of Usher syndrome, but this rare, inherited disorder causes hearing and vision loss in infants. The hearing loss can be mild to complete, and the vision slowly deteriorates over time. Scientists have identified 3 major types of Usher syndrome, characterized by how severe the hearing loss is. Treatment for this condition will depend on your child’s symptoms, age, health, as well as what type of Usher syndrome they have; early diagnosis of the condition, as well as proper management of it, can help improve your child’s overall quality of life.
What Is Usher Syndrome?

Named after Charles Usher, the British eye surgeon who identified the condition in 1914, Usher syndrome causes deafness because of an impaired ability in the inner ear and auditory nerves to transmit sound to the brain. The vision loss associated with it is caused by retinitis pigmentosa, a disorder that affects the retina, in which the light-sensing cells of the retina break down and cause vision loss over time. Blind spots develop first, and over time, they enlarge and merge to create tunnel vision.
How Common Is Usher Syndrome?
The National Institute of Health reports that Usher syndrome affects approximately 4 to 17 children out of 100,000 people, and accounts for about 50% of all hereditary deaf-blindness cases.
Causes Of Usher Syndrome
Usher syndrome is a genetic disease, passed down from parents to children when both parents are carriers of the gene. It is caused by mutations in several different genes that make up proteins involved in normal hearing, vision, and balance.
Usher syndrome is an autosomal recessive disorder, meaning:
- Both men and women are equally likely to have the disorder; it does not affect one gender more than the other.
- The condition occurs only when a child inherits both copies of the same gene from each parent.
Types and Symptoms of Usher Syndrome
There are 3 different types of Usher syndrome, each with a different level of severity. Types 1 and 2 are the most common, making up 95% of Usher syndrome cases. The types are characterized in the following ways:
- Type 1- Children with this type will have hearing loss or deafness at birth and severe balance issues. Babies will be able to sit without support, but at a later age than normal; they will also be late walkers, rarely walking before 18 months. Vision problems will begin before age 10, starting with difficulty seeing at night, and progressing quickly to total blindness. Many children with this type of Usher syndrome will not benefit from cochlear implants, an electronic device that can help people with hearing loss.

- Type 2– This type is characterized by hearing loss from birth and gradual vision loss that begins in either adolescence or adulthood. At birth, babies with type 2 Usher syndrome will have moderate to severe hearing loss, but normal balance. They will develop night vision problems as teenagers, with vision loss progressing more slowly and generally not resulting in total blindness. Children with this type will benefit from hearing aids.
- Type 3– People with type 3 Usher syndrome will experience hearing loss and vision loss beginning later in life. Babies will have normal hearing, with hearing loss beginning during late childhood or adolescence. Most children will have normal to near-normal balance, but may develop problems later in life. Night blindness starts in puberty, with blind spots occurring by late teens and total blindness by middle age. People with type 3 can benefit from hearing aids, as well.
Diagnosis
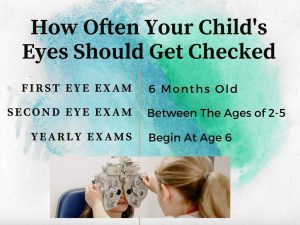
All newborn babies are screened for hearing problems when they are in the hospital, and if there is a problem, there will be follow-up testing. If there are any additional signs and symptoms of the syndrome, genetic testing might be done to find out if they have the Usher syndrome gene. Your child’s healthcare provider will also check your infant’s eyesight with the following tests:
- Electronystagmography (ENG)– A test that checks eye movements to help diagnose balance problems.
- Vision Testing– Physical examination of the retina to detect changes in blood vessels. Visual field testing will be done to measure the peripheral vision, as well as an electroretinogram (ERG), an exam based on the retina’s response to light, which confirms the diagnosis of retinitis pigmentosa.
Early diagnosis is important because it improves the likelihood of treatment success.
Treatment
Unfortunately, there is no known cure for Usher syndrome, but treatment will help manage hearing, vision, and balance problems. Early diagnosis is important, because it improves the likelihood of treatment success; treatment will depend on your child’s symptoms, age, and health, as well as how severe the condition is. Treatment can include:
- Cochlear implants
- Hearing aids
- Hearing or auditory training
- Use of American Sign Language
- Speech, physical, and occupational therapy
- Low vision support, such as magnifiers (hand held and for digital or computer use), large-print reading materials, or audio recordings.
- Orientation and mobility training to help with balance
- Vitamin A, which a long-term clinical trial from the National Eye Institute and the Foundation for Fighting Blindness suggests can slow the progression of retinitis pigmentosa.
- Counseling
Although there is no cure for Usher syndrome, children with the condition can live full, happy lives with ongoing treatment to help manage it. Seeing your child battling a condition like Usher syndrome is not easy, and the last thing you need in this situation is stress over how to pay the medical bills for treatments. But if you have the right health insurance plan, you won’t have to worry about medical bills, and will be able to simply focus on your child’s health. With EZ.Insure, it’s possible to get great affordable health insurance with the coverage you need: our agents work with the top-rated insurance companies in the country, and can compare all available plans in your area and provide you with quotes and information about each plan, for free. To get free instant quotes, simply enter your zip code in the bar above, or to speak to a licensed agent, call 888-350-1890.